What is high blood pressure?
Blood pressure is recorded with 2 numbers. The systolic pressure (higher number) is the force at which your heart pumps blood around your body.
The diastolic pressure (lower number) is the resistance to the blood flow in the blood vessels.
They’re both measured in millimetres of mercury (mmHg).
As a general guide:
- high blood pressure is considered to be 140/90mmHg or higher (or 150/90mmHg or higher if you’re over the age of 80)
- ideal blood pressure is usually considered to be between 90/60mmHg and 120/80mmHg
Blood pressure readings between 120/80mmHg and 140/90mmHg could mean you’re at risk of developing high blood pressure if you do not take steps to keep your blood pressure under control.
Everyone’s blood pressure will be slightly different. What’s considered low or high for you may be normal for someone else.
Your blood pressure
- heart disease
- heart attacks
- strokes
- heart failure
- peripheral arterial disease
- aortic aneurysms
- kidney disease
- vascular dementia
If you have high blood pressure, reducing it even a small amount can help lower your risk of these health conditions.
Check your blood pressure
The only way of knowing whether you have high blood pressure is to have a blood pressure test.
All adults over 40 are advised to have their blood pressure checked at least every 5 years.
Getting this done is easy and could save your life.
You can get your blood pressure tested at a number of places, including:
- at your GP surgery
- at some pharmacies
- as part of your NHS Health Check
- in some workplaces
You can also check your blood pressure yourself with a home blood pressure monitor.
Things that can increase your risk of getting high blood pressure
It’s not always clear what causes high blood pressure, but there are things that can increase your risk.
You might be more at risk if you:
- are overweight
- eat too much salt and do not eat enough fruit and vegetables
- do not do enough exercise
- drink too much alcohol or coffee (or other caffeine-based drinks)
- smoke
- do not get much sleep or have disturbed sleep
- are over 65
- have a relative with high blood pressure
- are of black African or black Caribbean descent
- live in a deprived area
Making healthy lifestyle changes can sometimes help reduce your chances of getting high blood pressure and help lower your blood pressure if it’s already high.
Treatment for high blood pressure
Doctors can help you keep your blood pressure to a safe level using:
- lifestyle changes
- medicines
What works best is different for each person.
Talk to your doctor to help you decide about treatment.
This patient decision aid (PDF, 132kb) can also help you to understand your treatment options.
Lifestyle changes to reduce blood pressure
These lifestyle changes can help prevent and lower high blood pressure:
- reduce the amount of salt you eat and have a generally healthy diet
- cut back on alcohol
- lose weight if you’re overweight
- exercise regularly
- cut down on caffeine
- stop smoking
Some people with high blood pressure may also need to take 1 or more medicines to stop their blood pressure getting too high.
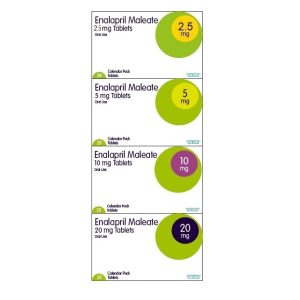
Medicines for high blood pressure
If you’re diagnosed with high blood pressure, your doctor may recommend taking 1 or more medicines to keep it under control.
These come as tablets and usually need to be taken once a day.
Common blood pressure medicines include:
- ACE inhibitors – such as enalapril, lisinopril, perindopril and ramipril
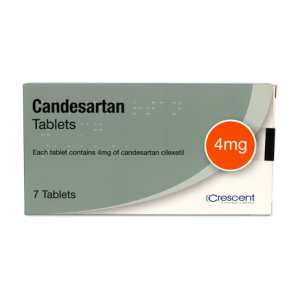
- angiotensin-2 receptor blockers (ARBs) – such as candesartan, irbesartan, losartan, valsartan and olmesartan
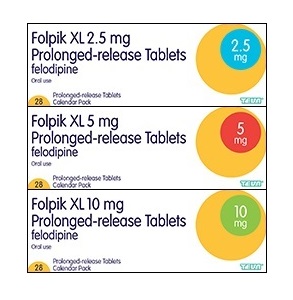
- calcium channel blockers – such as amlodipine, felodipine and nifedipine or diltiazem and verapamil
- diuretics – such as indapamide and bendroflumethiazide
- beta blockers – such as atenolol and bisoprolol
- alpha blockers – such as doxazosin
- other diuretics – such as amiloride and spironolactone
The medicine recommended for you will depend on things like how high your blood pressure is, your age and your ethnicity.
Causes
In most cases, it’s not clear exactly what causes high blood pressure. But there are things that can increase your risk.
Things that can increase your risk of getting high blood pressure
You might be more at risk if you:
- are overweight
- eat too much salt and do not eat enough fruit and vegetables
- do not do enough exercise
- drink too much alcohol or coffee (or other caffeine-based drinks)
- smoke
- do not get much sleep or have disturbed sleep
- are over 65
- have a relative with high blood pressure
- are of black African or black Caribbean descent
- live in a deprived area
Making healthy lifestyle changes can sometimes help reduce your chances of getting high blood pressure and help lower your blood pressure if it’s already high.
Known causes of high blood pressure
In about 1 in 20 cases, high blood pressure happens as the result of an underlying health condition or taking a certain medicine.
Health conditions that can cause high blood pressure include:
- kidney disease
- diabetes
- long-term kidney infections
- obstructive sleep apnoea – where the walls of the throat relax and narrow during sleep, interrupting normal breathing
- glomerulonephritis – damage to the tiny filters inside the kidneys
- narrowing of the arteries supplying the kidneys
- hormone problems – such as an underactive thyroid, an overactive thyroid, Cushing’s syndrome, acromegaly, increased levels of the hormone aldosterone (hyperaldosteronism), and phaeochromocytoma
- lupus – a condition in which the immune system attacks parts of the body, such as the skin, joints and organs
- scleroderma – a condition that causes thickened skin, and sometimes problems with organs and blood vessels
Medicines that can increase your blood pressure include:
- the contraceptive pill
- steroids
- non-steroidal anti-inflammatory drugs (NSAIDs) – such as ibuprofen and naproxen
- some pharmacy cough and cold remedies
- some herbal remedies – particularly those containing liquorice
- some recreational drugs – such as cocaine and amphetamines
- some selective serotonin-noradrenaline reuptake inhibitor (SSNRI) antidepressants – such as venlafaxine
In these cases, your blood pressure may return to normal once you stop taking the medicine or drug.
Diagnosis
Having this done is easy and could save your life.
Where to get a blood pressure test
You can ask for a blood pressure check. You do not have to wait to be offered one.
Blood pressure testing is available:
- at your GP surgery – by a GP, practice nurse, healthcare assistant or self-service machine
- at some pharmacies
- at an NHS Health Check appointment offered to adults aged 40 to 74 in England
- in some workplaces
- at a health event
You can also test your blood pressure at home using a home testing kit.
Having a blood pressure test
A stethoscope, arm cuff, pump and dial was normally used to measure your blood pressure, but automatic devices with sensors and digital displays are commonly used nowadays.
It’s best to sit down with your back supported and legs uncrossed for at least 5 minutes before the test.
You’ll usually need to roll up your sleeves or remove any long-sleeved clothing so the cuff can be placed around your upper arm.
Try to relax and avoid talking while the test is carried out.
During the test:
- you hold out one of your arms so it’s at the same level as your heart, and the cuff is placed around it – your arm should be supported in this position with a cushion or the arm of a chair, for example
- the cuff is pumped up to restrict the blood flow in your arm – this squeezing may feel a bit uncomfortable, but only lasts a few seconds
- the pressure in the cuff is slowly released and detectors sense vibrations in your arteries – a doctor will use a stethoscope to detect these if your blood pressure is measured manually
- the pressure in the cuff is recorded at 2 points as the blood flow starts to return to your arm – these measurements are used to give your blood pressure reading
You can usually find out your result straight away, either from the healthcare professional carrying out the test or on the digital display.
If your blood pressure is high, you may be advised to record your blood pressure using a 24-hour (ambulatory) monitoring kit or a home blood pressure monitoring kit to confirm whether you have high blood pressure.
Ambulatory (24-hour) blood pressure monitoring
Having a raised blood pressure reading in 1 test does not necessarily mean you have high blood pressure.
Blood pressure can fluctuate throughout the day. Feeling anxious or stressed when you visit your GP can also raise your blood pressure.
If you have a high reading, you may be asked to take some readings with a 24-hour monitor that checks your blood pressure throughout the day.
This will confirm whether you have consistently high blood pressure.
It’s known as 24-hour or ambulatory blood pressure monitoring.
Home blood pressure testing
Blood pressure tests can also be carried out at home using your own blood pressure monitor.
Like 24-hour or ambulatory monitoring, this can give a better reflection of your blood pressure.
It can also allow you to monitor your condition more easily in the long term.
You can buy a variety of low-cost monitors so you can test your blood pressure at home or while you’re out and about.
Measure your blood pressure twice a day, ideally in the morning and the evening, while you’re sitting down.
Each time take 2 readings, 1 minute apart. Continue to measure your blood pressure twice a day for 7 days.
Your doctor or nurse will use this information to work out your average blood pressure.
It’s important to make sure you use equipment that’s been properly tested.
The British Hypertension Society (BHS) has information about validated blood pressure monitors that are available to buy.
Understanding your blood pressure reading
Blood pressure is measured in millimetres of mercury (mmHg) and is given as 2 figures:
- systolic pressure – the pressure when your heart pushes blood out
- diastolic pressure – the pressure when your heart rests between beats
For example, if your blood pressure is “140 over 90”, or 140/90mmHg, it means you have a systolic pressure of 140mmHg and a diastolic pressure of 90mmHg.
As a general guide:
- high blood pressure is considered to be 140/90mmHg or higher (or an average of 135/85mmHg at home) – or 150/90mmHg or higher (or an average of 145/85mmHg at home) if you’re over the age of 80
- ideal blood pressure is usually considered to be between 90/60mmHg and 120/80mmHg, while the target for over-80s is below 150/90mmHg (or 145/85mmHg at home)
Blood pressure readings between 120/80mmHg and 140/90mmHg could mean you’re at risk of developing high blood pressure if you do not take steps to keep your blood pressure under control.
Treatment
When treatment is recommended
Everyone with high blood pressure is advised to make healthy lifestyle changes.
Whether medicine is also recommended depends on your blood pressure reading and your risk of developing problems such as heart attacks or strokes.
Your doctor will carry out some blood and urine tests, and ask questions about your health to determine your risk of other problems:
- if your blood pressure is consistently above 140/90mmHg (or 135/85mmHg at home), but your risk of other problems is low – you’ll be advised to make some changes to your lifestyle
- if your blood pressure is consistently above 140/90mmHg (or 135/85mmHg at home) and your risk of other problems is high – you’ll be offered medicine to lower your blood pressure, in addition to lifestyle changes
- if your blood pressure is consistently above 160/100mmHg – you’ll be offered medicine to lower your blood pressure, in addition to lifestyle changes
Lifestyle changes
There are some changes you could make to your lifestyle to reduce high blood pressure.
Some of these will lower your blood pressure in a matter of weeks, while others may take longer.
Try to:
- cut your salt intake to less than 6g (0.2oz) a day, which is about a teaspoonful – find out how you can reduce the amount of salt in your diet
- eat a low-fat, balanced diet – including plenty of fresh fruit and vegetables; get tips on eating more healthily
- be active – read some tips about getting more exercise
- cut down on alcohol – get tips on cutting down, including downloading a drinks diary and keeping track of your drinking
- lose weight – find out what your ideal weight is using the BMI healthy weight calculator and read advice about losing weight if you’re overweight
- drink less caffeine – found in coffee, tea and cola
- stop smoking – get help quitting
You can take these steps today, regardless of whether or not you’re taking blood pressure medicines.
In fact, by making these changes early on you may be able to avoid needing medicines.
Get more advice about lifestyle changes to prevent and reduce high blood pressure
Medicines for high blood pressure
Several types of medicine can be used to help control high blood pressure.
Many people need to take a combination of different medicines.
- if you’re under 55 years of age – you’ll usually be offered an ACE inhibitor or an angiotensin-2 receptor blocker (ARB)
- if you’re aged 55 or older, or you’re any age and of African or Caribbean origin – you’ll usually be offered a calcium channel blocker
You may need to take blood pressure medicine for the rest of your life. But your doctor might be able to reduce or stop your treatment if your blood pressure stays under control for several years.
It’s really important to take your medicine as directed. If you miss doses, it will not work as well.
The medicine will not necessarily make you feel any different, but this does not mean it’s not working.
Medicines used to treat high blood pressure can have side effects, but most people do not get any.
If you do get side effects, do not stop taking your medicine. Talk to your doctor, who may advise changing your medicine.
ACE inhibitors
Angiotensin-converting enzyme (ACE) inhibitors reduce blood pressure by relaxing your blood vessels.
Common examples are enalapril, lisinopril, perindopril and ramipril.
The most common side effect is a persistent dry cough. Other possible side effects include headaches, dizziness and a rash.
Angiotensin-2 receptor blockers (ARBs)
ARBs work in a similar way to ACE inhibitors. They’re often recommended if ACE inhibitors cause troublesome side effects.
Common examples are candesartan, irbesartan, losartan, valsartan and olmesartan.
Possible side effects include dizziness, headaches, and cold or flu-like symptoms.
Coronavirus advice
If you have coronavirus (COVID-19), or think you might have it, keep taking your blood pressure medicines as usual.
There is no clear evidence that taking angiotensin-converting enzyme (ACE) inhibitors or angiotensin-2 receptor blockers (ARBs) will cause complications.
Calcium channel blockers
Calcium channel blockers reduce blood pressure by widening your blood vessels.
Common examples are amlodipine, felodipine and nifedipine. Other medicines, such as diltiazem and verapamil, are also available.
Possible side effects include headaches, swollen ankles and constipation.
Drinking grapefruit juice while taking some calcium channel blockers can increase your risk of side effects.
Diuretics
Sometimes known as water pills, diuretics work by flushing excess water and salt from the body through your pee.
They’re often used if calcium channel blockers cause troublesome side effects.
Common examples are indapamide and bendroflumethiazide.
Possible side effects include dizziness when standing up, increased thirst, needing to go to the toilet frequently, and a rash.
You might also get low potassium and low sodium after long-term use.
Beta blockers
Beta blockers can reduce blood pressure by making your heart beat more slowly and with less force.
They used to be a popular treatment for high blood pressure, but now tend to be used only when other treatments have not worked.
This is because beta blockers are considered less effective than other blood pressure medicines.
Common examples are atenolol and bisoprolol.
Possible side effects include dizziness, headaches, tiredness, and cold hands and feet.
High blood pressure in older people
The target blood pressure reading for the over-80s is below 150/90 mmHg when it’s measured in the clinic or surgery, and below 145/85 mmHg for home readings.
While there are definite benefits from taking medicines to reduce blood pressure if you’re under the age of 80, it’s less clear it’s useful if you’re over 80.
It’s now thought that if you reach 80 while you’re taking medicine for high blood pressure, it’s fine to continue treatment provided it’s still helping you and is not causing side effects.
If you’re diagnosed with high blood pressure and you’re aged over 80, your doctor will also consider your other health risk factors when deciding whether to give you treatment for the high blood pressure.
Prevention
Healthy diet
Cut down on the amount of salt in your food and eat plenty of fruit and vegetables.
The Eatwell Guide highlights the different types of food that make up our diet, and shows the proportions we should eat them in to have a well-balanced and healthy diet.
Salt raises your blood pressure. The more salt you eat, the higher your blood pressure. Aim to eat less than 6g (0.2oz) of salt a day, which is about a teaspoonful.
Find out how to cut down on salt
Eating a low-fat diet that includes lots of fibre, such as wholegrain rice, bread and pasta, and plenty of fruit and vegetables also helps lower blood pressure.
Aim to eat 5 portions of fruit and vegetables every day.
Limit your alcohol intake
Regularly drinking too much alcohol can raise your blood pressure over time.
Staying within the recommended levels is the best way to reduce your risk of developing high blood pressure:
- men and women are advised not to regularly drink more than 14 units a week
- spread your drinking over 3 days or more if you drink as much as 14 units a week
Find out how many units are in your favourite drink and get tips on cutting down.
Alcohol is also high in calories, which will make you gain weight and can further increase your blood pressure.
Lose weight
Being overweight forces your heart to work harder to pump blood around your body, which can raise your blood pressure.
Find out if you need to lose weight with the BMI healthy weight calculator
If you do need to lose some weight, it’s worth remembering that just losing a few pounds will make a big difference to your blood pressure and overall health.
Get active
Being active and taking regular exercise lowers blood pressure by keeping your heart and blood vessels in good condition.
Regular exercise can also help you lose weight, which will also help lower your blood pressure.
Adults should do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity, such as cycling or fast walking, every week.
Physical activity can include anything from sport to walking and gardening.
Cut down on caffeine
Drinking more than 4 cups of coffee a day may increase your blood pressure.
If you’re a big fan of coffee, tea or other caffeine-rich drinks, such as cola and some energy drinks, consider cutting down.
It’s fine to drink tea and coffee as part of a balanced diet, but it’s important that these drinks are not your main or only source of fluid.
Stop smoking
Smoking does not directly cause high blood pressure, but it puts you at much higher risk of a heart attack and stroke.
Smoking, like high blood pressure, will cause your arteries to narrow.
If you smoke and have high blood pressure, your arteries will narrow much more quickly, and your risk of heart or lung disease in the future is dramatically increased.
PLEASE NOTE ALL THE INFORMATION ABOVE IS FROM THE NHS WEBSITE