Showing all 3 results
-
Sold By - British Chemist

Trimethoprim 200mg tablets
£12.99 inc. VAT Learn More -
Sold By - British Chemist

MacroBID (Nitrofurantoin) 100mg Prolonged-release Capsules
£14.99 inc. VAT Learn More -
Sold By - British Chemist
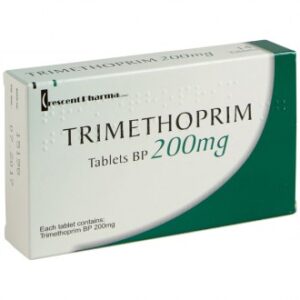
Trimethoprim 200mg tablets
£12.99 inc. VAT Learn More
Cystitis is inflammation of the bladder, usually caused by a bladder infection.
It’s a common type of urinary tract infection (UTI), particularly in women, and is usually more of a nuisance than a cause for serious concern.
Mild cases will often get better by themselves within a few days.
But some people experience episodes of cystitis frequently and may need regular or long-term treatment.
There’s also a chance that cystitis could lead to a more serious kidney infection in some cases, so it’s important to seek medical advice if your symptoms do not improve.
Signs and symptoms of cystitis
The main symptoms of cystitis include:
* pain, burning or stinging when you pee
* needing to pee more often and urgently than normal
* urine that’s dark, cloudy or strong smelling
* pain low down in your tummy
* feeling generally unwell, achy, sick and tired
Possible symptoms in young children include:
* pain in their tummy
* needing to pee urgently or more often
* a high temperature (fever) of 38C or above
* weakness or irritability
* reduced appetite and vomiting
When to see a GP
Women do not necessarily need to see a GP if they have cystitis, as mild cases often get better without treatment.
Try some self-help measures or ask a pharmacist for advice.
See a GP if:
* you’re not sure whether you have cystitis
* your symptoms do not start to improve within 3 days
* you get cystitis frequently
* you have severe symptoms, such as blood in your urine, a fever or pain in your side
* you’re pregnant and have symptoms of cystitis
* you’re a man and have symptoms of cystitis
* your child has symptoms of cystitis
A GP should be able to diagnose cystitis by asking about your symptoms.
They may test a sample of your urine for bacteria to help confirm the diagnosis.
What causes cystitis?
Most cases are thought to occur when bacteria that live harmlessly in the bowel or on the skin get into the bladder through the tube that carries urine out of your body (urethra).
It’s not always clear how this happens.
But some things can increase your risk of getting it, including:
* having sex
* wiping your bottom from back to front after going to the toilet
* having a thin tube inserted into the urethra to drain the bladder (urinary catheter)
* being younger than 1 or older than 75
* being pregnant
* using a diaphragm for contraception
* having diabetes
* having a weakened immune system
Women may get cystitis more often than men because their bottom (anus) is closer to their urethra and their urethra is much shorter, which means bacteria may be able to get into the bladder more easily.
How you can treat cystitis yourself
If you have been having mild symptoms for less than 3 days or you have had cystitis before and do not feel you need to see a GP, you may want to treat your symptoms at home or ask a pharmacist for advice.
Until you’re feeling better, it may help to:
* take paracetamol or ibuprofen
* drink plenty of water
* hold a hot water bottle on your tummy or between your thighs
* avoid having sex
* pee frequently
* wipe from front to back when you go to the toilet
* gently wash around your genitals with a skin-sensitive soap
Some people believe that cranberry drinks and products that reduce the acidity of their urine (such as sodium bicarbonate or potassium citrate) will help.
But there’s a lack of evidence to suggest they’re effective.
Treatments for cystitis from a GP
If you see a GP and they diagnose you with cystitis, you’ll usually be prescribed a course of antibiotics to treat the infection.
These should start to have an effect within a day or 2.
If you keep getting cystitis, a GP may give you an antibiotic prescription to take to a pharmacy whenever you develop symptoms, without needing to see a doctor first.
Your GP can also prescribe a low dose of antibiotics for you to take continuously over several months.
Preventing cystitis
If you get cystitis frequently, there are some things you can try that may stop it coming back.
But it’s not clear how effective most of these measures are.
These measures include:
* not using perfumed bubble bath, soap or talcum powder around your genitals (use plain unperfumed varieties)
* having a shower, rather than a bath (this avoids exposing your genitals to the chemicals in your cleaning products for too long)
* going to the toilet as soon as you need to pee and always emptying your bladder fully
* staying well hydrated (drinking plenty of fluids may help to stop bacteria multiplying in your bladder)
* always wiping your bottom from front to back when you go to the toilet
* emptying your bladder as soon as possible after having sex
* not using a diaphragm for contraception (you may wish to use another method of contraception instead)
* wearing underwear made from cotton, rather than synthetic material, such as nylon, and not wearing tight jeans and trousers
Drinking cranberry juice has traditionally been recommended as a way of reducing your chances of getting cystitis.
But large studies have suggested it does not make a significant difference.
Interstitial cystitis
If you have long-term or frequent pelvic pain and problems peeing, you may have a condition called interstitial cystitis.
This is a poorly understood bladder condition that mostly affects middle-aged women.
Unlike regular cystitis, there’s no obvious infection in the bladder and antibiotics do not help.
But a doctor may be able to recommend a number of other treatments to reduce your symptoms.
Cystitis can cause problems with peeing and make you feel unwell.
Symptoms of cystitis in adults
Cystitis in adults can cause:
* pain, burning or stinging when you pee
* needing to pee more often and urgently than normal
* feeling like you need to pee again soon after going to the toilet
* urine that’s dark, cloudy or strong-smelling
* pain low down in your tummy
* feeling generally unwell, achy, sick and tired
* blood in your urine
In adults, cystitis does not usually cause a high temperature (fever).
But if you have a temperature of 38C (100.4F) or above and pain in your lower back or sides, it may be a sign of a kidney infection.
Symptoms of cystitis in children
It can be difficult to tell whether a child has cystitis, because the symptoms can be vague and young children cannot easily communicate how they feel.
Possible symptoms of cystitis in young children may include:
* a high temperature (fever) of 38C (100.4F) or above
* weakness and tiredness
* irritability
* reduced appetite
* vomiting
Children with cystitis can sometimes also have symptoms usually found in adults, such as pain when peeing, peeing more often than normal and pain in their tummy.
When to see a GP
If you’re a woman who has had cystitis before, or you have mild symptoms that have lasted less than 3 days, you do not necessarily need to see a GP.
Cystitis is very common in women and mild cases often get better on their own.
Try some self-help measures or speak to a pharmacist if you need any advice about treating cystitis.
But you should see a GP if:
* you’re not sure if it’s cystitis
* your symptoms are severe
* your symptoms do not start to get better within 3 days
* you get cystitis frequently
* you’re pregnant
* your child has symptoms
* you’re a man
Children and men should always be seen by a GP if they have symptoms of cystitis, as the condition is less common and could be more serious in these groups.
Cystitis is not usually a cause for serious concern, but the symptoms can be similar to several other conditions, so it’s important to get a proper diagnosis if you’re not sure whether you have it.
Interstitial cystitis
You should see a GP if you have long-term or frequent pelvic pain and problems peeing, as you may have a condition called interstitial cystitis.
Causes
Cystitis is usually caused by a bacterial infection, although it sometimes happens when the bladder is irritated or damaged for another reason.
Bacterial infections
Most infections are thought to occur when bacteria that live harmlessly in the bowel or on the skin get into the bladder through the urethra (the tube that carries urine out of your body) and start to multiply.
Cystitis is much more common in women than men, probably because the anus (back passage) is closer to the urethra in women and the urethra is much shorter.
It’s not always obvious how the bacteria get into the bladder.
But some things can increase the risk of it happening, including:
* having sex
* wiping your bottom from back to front after going to the toilet
* having a urinary catheter (a thin tube inserted into the urethra to drain the bladder)
* using a diaphragm for contraception
What can increase your risk?
There are a number of things that can increase your chances of developing an infection in your bladder.
Some of these are outlined on this page.
Not being able to empty your bladder
If you’re unable to empty your bladder fully, any bacteria that get inside may not be flushed out when you go to the toilet and can multiply more easily.
You may not be able to empty your bladder fully if:
* you have a blockage in your urinary system, such as a bladder stone
* you’re pregnant, as the baby may be pressing on your bladder
* (in men) you have an enlarged prostate gland that presses on the urethra
Menopause
For women who have been through the menopause or are going through it, the lining of the urethra can shrink and become thinner because of a lack of the hormone oestrogen.
The natural balance of bacteria in the vagina may also change, which can allow potentially harmful bacteria to become more common.
This can make the urethra more vulnerable to infection, which could spread into the bladder.
Diabetes
You’re more likely to get cystitis if you have diabetes, a condition where the level of sugar in your body becomes too high.
High levels of sugar in your urine can provide a good environment for bacteria to multiply, so any bacteria that get into the bladder are more likely to cause cystitis.
Other causes of cystitis
Cystitis can also be caused by damage or irritation to the urethra and bladder.
This can be the result of:
* friction from sex
* chemical irritants, such as those in perfumed soap or bubble bath
* damage caused by a catheter or surgery on your bladder
* radiotherapy to your pelvis or treatment with certain chemotherapy medicines
* a woman’s genitals having been deliberately cut or changed for cultural, religious and social reasons (an illegal practice called female genital mutilation, or FGM)
Cystitis has also been linked to recreational use of the drug ketamine.
Mild cystitis will usually clear up on its own within a few days, although sometimes you may need to take antibiotics.
See a GP for advice and treatment if:
* you’re not sure whether you have cystitis
* your symptoms don’t start to improve within 3 days
* you get cystitis frequently
* you have severe symptoms, such as blood in your urine
* you’re pregnant and have symptoms of cystitis
* you’re a man and have symptoms of cystitis
* your child has symptoms of cystitis
Women who have had cystitis before or who have had mild symptoms for less than 3 days don’t necessarily need to see a GP, as mild cases often get better without antibiotics.
You can try some self-help measures or ask a pharmacist for advice.
Things you can try yourself
If you have had cystitis before and don’t feel you need to see a GP, or had mild symptoms for less than 3 days, the following advice may help to relieve your symptoms until the condition clears up:
* take over-the-counter painkillers, such as paracetamol or ibuprofen (always read the medicine information leaflet beforehand to check whether you can take it, and check with a pharmacist if you’re not sure)
* drink plenty of water (this may help flush the infection out of your bladder and some people find it helpful, although it’s not clear how effective it actually is)
* don’t have sex until you’re feeling better as it may make the condition worse
Some people believe drinking cranberry juice or using products that lowers the acidity of their urine (such as sodium bicarbonate or potassium citrate) reduces their symptoms, but there’s a lack of evidence to suggest they’re effective.
These products also aren’t suitable for everyone. Check with a GP or pharmacist before trying them if you’re taking any other medication.
Antibiotics
In some cases, a GP may prescribe a course of antibiotics. This will usually involve taking a tablet or capsule 2 to 4 times a day for 3 days.
For some women, they’ll be prescribed for 5 to 10 days.
Antibiotics should start to have an effect quite quickly. Go back to your GP if your symptoms haven’t started to improve within a few days.
Most people won’t have any side effects from antibiotic treatment, but possible side effects can include feeling or being sick, itching, a rash and diarrhoea.
If cystitis keeps coming back
If you keep getting cystitis (recurrent cystitis), a doctor may prescribe stand-by antibiotics or continuous antibiotics.
A stand-by antibiotic is a prescription you can take to a pharmacy the next time you have symptoms of cystitis without needing to visit a GP first.
Continuous antibiotics are taken for several months to prevent further episodes of cystitis.
These may be prescribed:
* if cystitis usually occurs after having sex (you may be given a prescription for antibiotics to take within 2 hours of having sex)
* if cystitis isn’t related to having sex (you may be given a low-dose antibiotic to take for a trial period of 6 months)
Your doctor may also recommend some measures you can take to prevent cystitis, although it’s not clear how effective these are.
Please note this information is from the NHS website.

